Inflammatory Bowel Disease
What is Inflammatory Bowel Disease?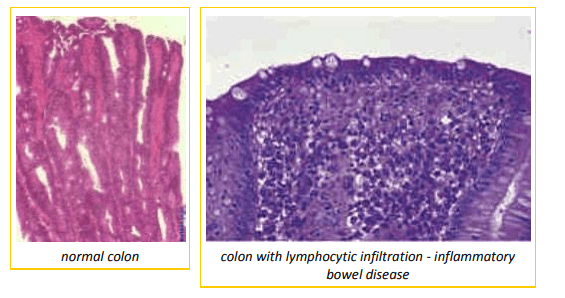
Inflammatory bowel disease (IBD) refers to the condition that results when cells involved in inflammation and immune response are called into the lining of the GI tract. This infiltration thickens the bowel lining and interferes with absorption and motility (the ability of the bowel to contract and move food). With abnormal ability to contract and abnormal ability to absorb, the bowel’s function is disrupted. Chronic vomiting results if the infiltration is in the stomach or higher areas of the small intestine. A watery diarrhea with weight loss results if the infiltration is in the lower small intestine. A mucous diarrhea with fresh blood (colitis) results if the infiltration occurs in the large intestine. Of course, the entire tract from top to bottom may be involved. Many people confuse inflammatory bowel disease with irritable bowel syndrome, a stress-related diarrhea problem. Treatment for irritable bowel is aimed at stress; it is a completely different condition from IBD.
It is important to consider IBD to be an immunologic reaction to some kind of immunologic stimulation. In other words, IBD is more of a symptom than an actual disease in and of itself. In a perfect world, the source of the stimulation, be it dietary, bacterial, or parasitic, could be removed and the patient would return to normal without further treatment. Unfortunately, in most cases treatment centers on managing the immunologic reaction and consequent symptoms.
Why would the Veterinarian Think My Pet Might have Inflammatory Bowel Disease?
A little vomiting or diarrhea here and there seems to be pretty standard for pet dogs and cats. After all, cats groom themselves and get hairballs. Dogs eat all sorts of ridiculous things they aren’t supposed to. Still, many owners notice that their pets seem to have vomiting or diarrhea a bit more often than it seems they should. It might be subtle where one notices that one is cleaning up a hairball or vomit pile rather more frequently than with previous pets or it could be the realization that one has not seen the pet have a normal stool in weeks or months. Typically, the animal doesn’t seem obviously sick. Maybe there has been weight loss over time but nothing acute. There is simply a chronic problem with vomiting, diarrhea or both. Inflammatory bowel disease is probably the most common cause of chronic intestinal clinical signs and would be the likely condition to pursue first.
How is Inflammatory Bowel Disease Diagnosed?
The first step in pursuing any chronic problem is a metabolic database. This means a basic blood panel and urinalysis to rule out biochemically widespread problems (such as liver disease or kidney disease) that could be responsible for the signs. Since inflammatory bowel disease is localized to the GI tract, such a database is usually normal (but might express a general inflammatory response in the blood or a loss of blood proteins as often there is a leaking of albumin (an important blood protein) from the intestine into the bowel contents).
Radiographs may also be a good idea to rule out growths in the abdomen or tumors that could be accounting for the chronic problems.
A trial of a simple medication such as metoclopramide (Reglan) or metronidazole (Flagyl) is often used to see if there is symptomatic relief.
Broad spectrum deworming is often performed and sometimes more extensive parasite testing is done, especially if the patient is under age one year or has a history of living with numerous other animals. Typical parasites to rule out for patients with diarrhea include: Giardia, cryptosporidium and possibly Tritrichomonas. In younger patients bacterial infections, such as with Campylobacter and Salmonella, are also commonly tested.
If this kind of non-invasive testing is not revealing, then the definitive test for inflammatory bowel disease is needed: a biopsy. Tissue samples must be harvested from several areas of the GI tract. This can be done either surgically or via endoscopy.
Endoscopy involves the use of a skinny tubular instrument (an endoscope) which has a tiny fiber optic or video camera at the end. The endoscope is inserted down the throat, into the stomach and into the small intestine where small pinches of tissue are obtained via tiny biting forceps. If the large intestine is to be viewed, a series of enemas is needed prior to the procedure as well as a relatively long fast. The endoscope is inserted rectally and again tissue samples are harvested. The advantage of this procedure over surgery is that it is not as invasive as surgery. Patients typically go home the same day. Disadvantages are expense (often referral to a specialist is necessary) and the fact that the rest of the
abdomen cannot be viewed. Growths that are seen via endoscopy cannot be removed at that time and a second procedure typically must be planned whereas, if surgical exploration is used to obtain the biopsy, any growths can also be excised at that time.
Surgical exploration may also be used to obtain samples. The recovery afterwards is typically a couple of days though some patients bounce back immediately. With surgery, other organs can also be sampled and abnormal sections of tissue can be removed. Surgery tends to be more expensive than endoscopy but this depends on the recovery period. Often these two procedures work out to be of similar expense.
Tissue samples obtained are processed by a laboratory and analyzed. The infiltration of inflammatory cells is graded as mild, moderate, or severe and the type of cells involved in the inflammation are identified.
What Causes It?
Unfortunately, the causes of IBD are not well understood. Usually, a cause is not found. The basic theory
is that “something” is leading to a chronic stimulus of inflammation. This could be an allergy against a food protein, the continuing presence of a parasite, inflammatory products produced by the normal bacteria living in the intestine or there may be an underlying problem with the immune system in affected individuals. Obviously, there may be different causes in different individuals or a combination of the possibilities listed working together. Most of the time an extensive search for the underlying cause is not made because of expense.
What are Other causes of Chronic Vomiting or Diarrhea?
It is important to rule out parasitism as best as possible in cases such as these. A fecal flotation for worms is a good idea. Parasites such as whipworms or giardia may be difficult to detect so a short course of treatment to rule them out might also be a good idea, especially in a dog.
Pancreatic enyzyme insufficiency or chronic pancreatic inflammation (pancreatitis) might cause chronic vomiting or diarrhea. Blood tests are required to rule out these possibilities. Pancreatic enzyme insufficiency is an especially important problem in German Shepherd dogs.
More serious causes of chronic gastrointestinal complaints might include intestinal cancer (especially lymphosarcoma/lymphoma), fungal infection infiltrating the GI lining, or a lymphatic condition called lymphangiectasia. A biopsy will differentiate inflammatory bowel disease from these other conditions. If substantial blood proteins are being lost through the GI tract biopsy to rule out these conditions is particularly important and aggressive therapy will be necessary.
An infection in the stomach with a bacterium called Helicobacter is associated with IBD, but we do not know enough to establish which is the cause and which is the effect. Helicobacter infection can lead to ulceration and inflammation, compounding the problems of the inflammatory bowel disease. Treatment is necessary for this type of infection.
More serious causes of chronic gastrointestinal complaints might include intestinal cancer (especially lymphosarcoma/lymphoma), fungal infection infiltrating the GI lining (histoplasmosis), or a lymphatic condition called lymphangiectasia. A biopsy will differentiate IBD from these other conditions.
How is it Treated?
The cornerstone of treatment for inflammatory bowel disease is suppression of the inflammation. In milder cases of large intestinal inflammatory bowel disease, the immunomodulating properties of metronidazole (Flagyl) might be adequate for control but usually prednisone is needed. Prednisone will work on inflammatory bowel disease in any area of the intestinal tract. In more severe cases, stronger immune suppression is needed (as with cyclosporine or azathioprine). Higher doses are usually used in treatment at first and tapered down after control of symptoms has been gained. Some animals are able to eventually discontinue treatment or only require treatment during flare-ups. Others require some medication at all times. Long-term use of prednisone should be accompanied by appropriate periodic monitoring tests due to the immune suppressive nature of this treatment.
Dietary manipulation may also be helpful in the management of inflammatory bowel disease depending on the patient’s interest in newer foods.
In cats, prednisolone seems to be more effective than prednisone, the difference in these two medications being that prednisone must be activated within the body and prednisolone is already active. Cats also do not tolerate azathioprine and typically receive chlorambucil.
In cases where it is particularly important to spare the patients from the side effects of long-term steroids a medication called budesonide can be used. This medication is not readily absorbed from the GI tract and serves as a topical treatment for the lining of the intestine.
Dietary manipulation may also be helpful in the management of inflammatory bowel disease depending on the patient’s interest in newer foods. See below for more details.
How Can Diet be Used to Treat IBD?
The first step in dietary management of IBD is fat restriction. Fat prolongs the time food spends in the stomach, which tends to promote nausea. There can also be undesirable interactions with fats and the bacteria of the intestine.
Beyond this there are several dietary approaches to IBD.
Hypoallergenic Diet
Here a novel or hydrolyzed protein-based diet is used, the idea being that some of the immunologic stimulation may be from diet. If the patient is on a diet he/she cannot possibly be allergic to then recovery is possible. Sometimes a sacrificial protein diet is used during the healing process with the expectation that the patient may become allergic to the treatment diet and will be switched to another hypoallergenic diet at the end of the diet trial. Food allergy is definitely a cause of IBD. For more information on hypoallergenic diets, see our food allergy information.
Low Residue Diet
Here a diet that is especially easy to digest and absorb is used. These are typically prescription intestinal diets.
High Fiber Diet
Insoluble fibers have been helpful in IBD. They increase fecal bulk which stimulates more normal motility from the intestine. Slower stool passage results which enhances water absorption. Adding oat bran to the hypoallergenic diet may be helpful.
For more specific information on the use of fiber, review colitis.
Is it at all Reasonable to just Try Treatment and Skip the Expensive Diagnostics?
Possibly. The problem with the prednisone or prednisolone trial involves the possibility of intestinal lymphosarcoma (also called lymphoma). This is a type of cancer that produces chronic diarrhea or vomiting just as IBD can. Lymphoma is temporarily responsive to prednisone but the response is shortlived. Exposure to prednisone will make the lymphoma much more difficult to diagnose should biopsies be obtained later. Plus exposure to prednisone can lead to resistance to other medications. (This is less of a problem for cats, but in dogs even a few days of prednisone can make a lasting remission impossible to achieve.)
In short, if you try prednisone or prednisolone without confirming a diagnosis, harm can be caused should the pet have lymphoma instead of IBD.
Inflammatory bowel disease continues to be a common cause of chronic intestinal distress in both humans and animals. Research for less invasive tests and for newer treatments is ongoing.
Date Published: 1/1/2001
Date Reviewed/Revised: 3/7/2012
