- Anti-microbial Resistance (AMR)
- Bloat
- BVD
- Calf Colostrum
- Calf Disbudding
- Dry Cow Therapy
- Calf Scours
- Lameness
- Facial Eczema
- Mycoplasma Bovis
- Mastitis
- Nitrate Poisoning
- Pink Eye
- Poisoning
- Pregnancy Testing
- Salmonella
- Thelieria
- Welfare
- Zoonoses
Anti-Microbial Resistance (AMR)

One of the amazing but common place tech things that I still find really cool is the multi-participant webinar. The NZVA recently hosted one to coincide with Anti-Microbial Resistance (AMR) Awareness Week, and various speakers raised some really good points and insights:
An article in the Lancet modeled that 35 million deaths globally would be attributable to AMR by 2030, with an impact on food supply and health costs. The WHO and the UN have made this issue a priority. The One Health model underlines the connection between people, animals and the environment. Antimicrobial resistance can transfer between bacteria across these lines. We have a role and responsibility in this space because it is included in free trade agreements with the EU and the UK.
So, what can we do as vets and farmers?
- Design an Animal Health Plan which details Preventative Health Measures
- Vaccination programs are a simple example –
we should be considering routine vaccination for Salmonella as well as Lepto - Only use antibiotics when needed
- Teat Seal and anti-inflammatories have increasingly been taken up as alternatives
- Foot-trimming and hoof blocks
- Nutritional scours are best treated with fluids, electrolytes
- Colostrum management including brix-testing to identify the Gold stuff,
and blood testing calves to monitor colostrum uptake - Milk cultures on cows with mastitis or high cell count, either in clinic or the Mastatest system.
No growth or non-toxic gram negative infections may best be treated with anti-inflammatories. - Wearables / collars / good cow monitoring will identify cow health issues early
- Accurate feed budgets to minimize stress, monitoring transition period
- Milking Management Visits to check teat scores and monitor milking health to reduce mastitis risk
- BCS and Locomotion Scoring to identify issues and get ahead of them early
If we reduce unnecessary use of antimicrobials, we increase the likelihood of them working when we need them!

- CONTROL
Control of bloat includes pasture and grazing management, anti-bloat capsules, anti-foaming agents and as a last resort the old emergency rumenotomy (stab!). - GRAZING MANAGEMENT
Higher dry matter levels, hay feeding, longer rotations, species of plants grazed, continuous grazing and careful fertilizer application can all greatly aid in reducing bloat. - ANTI-FOAM AGENTS
Include: oils and fats, marlophens and detergents (alcohol ethoxylates and pluronics). These agents act by breaking down an already formed stable foam. Fats, oils and marlophens are safer, but slow to work and short-lived. Detergents are faster acting, and much more persistent but can be toxic if overdosed or given to calves. - RUMEN MODIFIERS
These prevent a stable foam forming by changing the proportions of microorganisms in the rumen and hence the way feed is broken down. These compounds also have the added benefit of increasing feed conversion efficiency.
METHODS OF CONTROL
SLOW RELEASE CAPSULES (Monensin)
- Give 100 days cover.
- Generally cost effective.
- Low time input; more peace of mind.
- Need to administer 5-7 days prior to expected bloat challenge.
- May need to use an anti-foaming agent as well during very severe challenge or in 1st 5-7 days.
- Toxic to dogs and horses.
DRENCHING (TERICS, PLURONICS)
- Can vary dose rates according to the challenge.
- Twice daily in moderate – severe challenge.
- Unsuitable in some sheds.
- Take care not to overdose.
- Never use detergents in calves – use oils.
- Low price option.
- High labour input.
PASTURE SPRAYING
- Use in the dry period, for heifers, in non-drenching sheds etc.
- Made of oils, emulsified oils and fats, detergents with sticking agent.
- Higher dose of active ingredient therefore higher cost.
- Must spray total area.
- Can only use 12-24 hours ahead.
- Break-feed. No back-grazing.
- High labour input.
BVD – Common, costly and controllable.
BVD (Bovine Viral Diarrhoea) is one of the most common and costly diseases in New Zealand cattle.
The problem with BVD is that many of the losses it causes are not obvious; your cattle may have this disease and you may not be aware of it. In NZ about 15%-20% of dairy herds and 65% of beef herds are infected with BVD, and most beef and dairy herds will be infected at some point in time. The infection causes scouring and ill thrift in young stock, infertility, increased somatic cell counts and production losses in adult cattle.
When breeding cows are infected you probably won’t see any obvious ill-health effects in that breeding cow. However the effects on fertility and on the unborn calf are profound, including low in-calf rates, abortion, stillbirths, birth of “dummy calves” and the birth of persistently infected (PI) carriers of BVD virus.
The economic impact in dairy herds has been estimated at between $35 and $87 per cow per year in an infected herd. In beef herds economic losses are associated with ill thrift in young stock and on average, a 5% increase in empty cows.
Control of BVD is relatively simple, involving testing and culling of PI cattle, biosecurity measures to keep the virus out, and vaccination. Advances in laboratory diagnosis mean that it is now simpler and more cost effective to diagnose and eradicate BVD from a herd than ever before. Tests can be done on individual animals and on bulk milk samples. Biosecurity measures include testing of all incoming stock onto the farm. An important group to test is breeding bulls – we recommend that all breeding bulls are tested for BVD virus before purchase. Vaccination may be recommended by your vet as a simple and cost effective measure for controlling BVD on your farm. Ultravac® BVD has been proven to be highly effective at preventing losses due to BVD, including protecting the foetus and preventing the birth of carrier (PI) cattle .
The first step in BVD control is to determine the BVD status of your farm, through appropriate testing. Then it’s a matter of working together with your vet to put in place a long term management plan for control of the disease.
For further information on BVD control, talk to your vet today.
BVD infections can be disruptive and costly. Finding and controlling PI (Persistently Infected) stock on your farm is an essential start.

Other important things to remember are having:
- Clean, dry pens with solid partitions
- Regular disinfection
- Hospital pens for sick calves, and
- Boot disinfectant by the doors.
Introduction
Cattle with horns are dangerous to people and other animals and are removed for welfare reasons. The process of removing horns in young cattle is referred to as calf disbudding or calf dehorning. This is a service provided to our farm clients and lifestyle block holders by Cambridge Veterinary Services.
Procedure
Calves are generally disbudded by a team of qualified staff including a veterinarian, when they are between 2-6 weeks of age (less stressful to the calf and the handler). The procedure involves heavily sedating all calves and the administration of local anaesthetic to the surrounding area. Additional pain relief in the form of NSAIDs can also given upon request. This method of disbudding ensures the horn buds are removed effectively at the correct time, with a minimum of pain and discomfit to the animal.
While the calves are sedated, ear tags can be easily applied, navels can be checked for infection and extra teats that will interfere with future milking can be removed. Calves can also be given their first sensitizing dose of clostridial 5 n 1 vaccine.
New Welfare RegulationsThe new dehorning welfare regulations come into effect this year (MONTH). Essentially this means local anaesthetic must be used for disbudding or dehorning animals of any age. For most of our clients who use us for dehorning, it’s business as usual. However if you want to do the dehorning yourself, we need to do a certification process with you whereby you receive training on how to administer the local etc, and are observed doing the job to a satisfactory standard. Thereafter is a requirement for annual re-certification on-farm. An RVM authorization is issued to allow local to be held on farm. The volume of local dispensed and used is limited and must be recorded for audit. Likewise all procedures need to be recorded.
Trial work suggests giving an anti-inflammatory as well as local is beneficial to the calves .
It may require a bit more planning for dehorning contractors. They need to do a similar procedure but the local is issued under VOI because the animals are not under their immediate care. Also the product can only be purchased from the veterinary business which issued the VOI, and used within a specified area.
Disbudding Calves, topical local anaesthetic and effects on pain
VetEnt and Massey conducted a study in which they compared different treatments for disbudding 364 calves (2-6 weeks). Calf behaviour and pain sensitivity over the next 24 hours were monitored, and weight gain recorded.
All calves had a local cornual nerve block, as is now a legal requirement and which generally wears off in 2-3 hours. Half were sedated, half restrained in a crate.
Both these groups were then further divided into 3:
- Nothing further
- Meloxicam injection before disbudding
- Topical anaesthetic antiseptic gel spray applied to the horn bud wounds afterwards
The calves were then assessed for the frequency of ear flicks, head shakes, head scratches and pain sensitivity of the wound (how much pressure can be applied). Additionally calves were weighed before disbudding and 7 & 28 days afterwards.
Conclusions
- Sedation reduced pain (ear flicks and sensitivity to pressure).
- Additional treatment with either meloxicam or TriSolfen further improved behavioural responses and pain sensitivity.
- Average daily weight gain at 7 days was 0.14kg/d better for calves that had sedation plus metacam, and 0.09kg/d better for sedated calves at 28 days.
We have moved into a new age – the Post Antibiotic Era.
Well, maybe not, but we are certainly part of the movement to reduce, replace and rationalize antimicrobial usage so that we minimize the spread of drug resistant bacteria to people. The NZVA states that by 2030 we should no longer need antibiotics to maintain animal health. This does not mean we won’t be able to treat sick animals, rather it is an aspirational aim to have better preventative health programs, management and husbandry in place so we don’t need to use antibiotics prophylactically. You can see our industry/profession has already made inroads with this, such as the work and recommendations done on colostrum management and pen hygiene to maximize calf health, and the focus on drying off practices and an increasing use of teat sealants.
However, this most affects us with antibiotic dry cow therapy. Blanket DCT is no longer permitted; we are allowed to treat high SCC cows or those with a mastitis profile, but “clean” cows need to be managed through dry off procedure/teat sealants/environmental management/ monitoring. This means that we need to identify high/low cell count cows. A herd test is the best solution to this, otherwise the cows could be RMT’d.
The other side of the coin is the Traffic Light Categorization of antimicrobials. We are trying to use/prescribe less Red antibiotics, as these are considered critical for human health. There are a limited number of choices to be fair, but it is something we need to address nonetheless.
The MPI report “Antibiotics Sales Analysis” details the National consumption of antibiotics in the animal & horticultural sector for 2017. Interestingly it shows that 58% was used in medicated feeds, 23% of sales were for injectable, 12% intra-mammaries, and half of all antibiotics were used in the pig and poultry industry. Alarmingly, the sale of products “critical to human health” went up for 4 of the 5 drugs.
Treatment of Calf Scours – Made easy
Diarrhoea (scours) is the single most important disease of the neonatal calf and is responsible for the greatest economic losses in this age group.
Calf scours is a complex disease; the causes of which are well known (nutritional, rotavirus, E.coli, cryptosporidia, salmonella, coccidia, corona). The resulting diarrhoea leads to a loss of electrolytes and large volumes of water in the faeces, damage to the lining of the gut with reduced milk absorption and changes to the gut bacteria.
Irrespective of the cause of diarrhoea, electrolyte replacement therapy remains the primary treatment of choice. Antibiotics & gut protectants (of which there are many) play a supportive role.
TREATMENT
Scouring calves can be divided into 4 groups according to the degree of dehydration present;
Bright and alert with a strong suckle reflex – group 1
• Weak suckle reflex, standing or sitting quietly – group 2
• No suckle reflex, depressed, unable to stand – group 3
• Collapsed, lying on side, no suckle reflex, death imminent – group 4
The presence or absence of the suckle reflex will primarily determine which route the fluid will be given; orally or intravenously.
Death generally arises when fluids/electrolytes are given too little or too late.
Group 1 & Group 2 Calves
Oral replacement therapy is highly effective with 95% of calves surviving if fluid therapy is administered early and continued until full recovery. Fluids and electrolytes can be given orally either by a bottle/teat system or oesophageal feeder (see below for instructions on how to use the oesophageal feeder).
Aim to give 7-10L’s/day divided into 2 litre feeds – that’s 4-5 feeds/day! This sounds like a lot of fluid (and work) but remember we need to replace fluid lost through ongoing diarrhoea, replace the deficits already incurred and give the calf fluid for daily maintenance requirements.
There are a number of excellent commercially available, carefully balanced electrolyte replacers on the market for treatment of calf scours. All of these products contain glucose or a similar material, sodium chloride and other electrolytes. Giving straight water does not work. Consult with your veterinarian regarding the appropriate oral electrolyte product for your needs. Always follow the label mixing instructions–do not add too much powder to the solution as this may further harm the calf and unnecessarily add to the cost of treatment.
Milk is also required to provide the calf with an energy source but milk should not be mixed with the electrolytes as this may affect curd formation within the abomasum. A feeding interval of 3 hours is needed between electrolyte/milk feeds. The table below can be used as a guide to fluid therapy.
Group 3 & 4 Calves
Once the suckle reflex has been lost and the calf is down IV fluid therapy is therapy is essential. Contact your vet immediately for further assistance. IV fluid therapy can improve the status of the animal quickly (if administered early). This will return the animal to a group 2 calf and fluid therapy can continue with an oesophageal feeder.
Fluid therapy continues until the scour has resolved.
DIAGNOSTICS
Faecal samples are often requested/collected from sick calves to differentiate a nutritional scour from an infectious scour and to determine the causative agent. By identifying the pathogen responsible for disease we are able to recommend product specific treatment options, effective disinfectants & vaccination programs. We can also develop a plan and implement strategies to minimise further exposure and disease. Advances in laboratory diagnostic tools means we are able to have results back, in many cases, on the same day.
SUPPLEMENTARY TREATMENT PRODUCTS
Many products exist on the market that aid in calf scour recovery and as suggested should only be used to supplement therapy.
Appropriate rehydration is essential.
Antibiotics: The use of antibiotics (scour ban, pink tablets, injectables etc) for calf scours is controversial however if blood is present in the faeces antibiotics are generally warranted. Speak to your vet.
Binding agents: Binding agents are generally some type of plant fibre/pulp that viruses and bacteria will “stick” to. In this way the infectious agents will preferentially bind to the fibre instead of the intestinal wall and will be passed out in the diarrhoea. The binders also slow down the rate of passage of fluid through the gut, giving the intestine more time to absorb water back into the calf’s system.
Antibody powders: are now available for scours caused by either Rotavirus and/or Cryptosporidia. It can be used to prevent and treat specific calf scours however its use is only justified upon a confirmed faecal diagnosis of either one or both of these pathogens.
Products are also available that reduce the severity of scours and the excretion of infective eggs into the environment. Talk to your vet.
WHEN DO I NEED HELP?
If your treatment methods are not working, contact your veterinarian immediately for additional help. If more than 5% of your calves are scouring and require treatment, you need help. If death is greater than 2% due to calf scours contact your veterinarian. Your veterinarian can submit refrigerated (not frozen) faecal samples to the lab and receive answers, in most cases, on the same day. Freshly dead calves can also be examined to determine the cause of the diarrhoea and to aid in determining those factors needed for prevention and treatment in your herd.
If you wish to discuss the management of calf scours further, require additional assistance, or need advice on animal health issues feel free to call your vet.
NURSING CARE AND PREVENTION
The most important aspect of control focuses on minimising predisposing factors and implementing strategies to prevent them from occurring on farm.
- Good colostrum management is critical to prevent disease– 2L’s of colostrum by bottle or feeder within 12 hours of birth.
- Prompt identification of sick calves, removal to hospital pens, and administration of effective, vigorous treatment. Don’t forget calf covers for warmth.
- Establish an isolated ‘hospital’ shed to minimise the spread of disease from infected animals. Once the calf has recovered it does not go back into the ‘healthy’ shed.
- Care should be taken to prevent the risk of personnel carrying contaminated material from the sick calves to animals in healthy pens. Consider establishing foot baths. Treat & feed the calves in the hospital pen last.
- Meticulous attention to hygiene is critical. All utensils used for feeding calves and storing milk should be thoroughly cleaned on a regular basis. Utensils used with sick calves should not be used for healthy calves.
- Avoid mixing calves of different ages. Use an all in/all out system.
- Clean (with an effective, safe and appropriate disinfectant) spraying the pens on a weekly basis and/or spell pens between batches of calves.
- Provide clean, fresh drinking water in drinkers that cannot become contaminated with faeces.
- Handling of CMR and provision of high quality compound feed and roughage is important.
- Provision of appropriate housing.
- Clean, new bedding annually.
- Vaccines are available for some pathogens – discuss with your vet
HOW TO USE AN OESOPHAGEAL FEEDER
An oesophageal feeder is a long flexible, plastic tube that screws onto a larger plastic container that holds the electrolytes. Prior to passing the feeder, always make sure the probe and the container are thoroughly clean (wash it after each use so it is clean for the next time).
- When administering the electrolyte fluid make sure it is at body temperature 35-40 degrees.
- Position the calf so that it is either standing or sitting up on its chest.
Gently lift the animals head up to insert the tube. If the calf struggles, lift the front end up so it is sitting on its haunches; you can restrain the calf easily that way while you lift its head to insert the tube. If the calf is standing, back it into a corner (or have someone hold its back end), step over its back so you can hold the head and neck between your legs, and pull the head up with one hand under the lower jaw—so you can insert the tube with your other hand. - Gently put the tube into the side of the mouth. This is easier (and easier on the calf) than trying to force it into the front. Then aim it straight and slide it over the tongue to the back of the mouth and into the throat. The calf should swallow it as you move it back and forth and apply gentle pressure. Make sure the tube is not forced into the windpipe; the calf must be given a chance to swallow as it is pushed down. Stop pushing for an instant and place your fingers on the outside of the neck (front of the throat), to determine where the tube is going. You can feel or see the bulb end of the tube slip down the throat and into the oesophagus.
- If you can see or feel the bulb (above the windpipe), you know it’s in the proper place and it’s safe to continue pushing the tube farther down. If you can’t see or feel it, or the calf is coughing, or there are puffs of air coming out your end, it’s in his windpipe; you must take it out and start over. Be sure it’s in the oesophagus and fully inserted (the bulb down close to the stomach) before you tip up the container or release the fluid into the tube. Hold the calf so it can’t struggle—or the tube may come partway out and allow fluid to get into the windpipe. Once positioned, the container can be lifted and the entire contents can be allowed to drain into the rumen.
New research (2018) on lameness in dairy cows has shown the importance of preventing the first lifetime lameness incident.
Jon Huxley is the new head of the Massey Vet School (another outstanding 1990s graduate from London!) and he brings a wealth of knowledge, research and enthusiasm. He recently outlined a change in our understanding of the progress of lameness. If a cow becomes lame, she grows little spurs on the sole of her toe bone which impacts on the cells below that grow sole horn. So then you get haemorrhage and weak sole which predisposes to lameness and the cycle continues….The good news is that trimming or using cowslips (thus relieving the pressure on those hoof producing cells) has a very beneficial effect.
Other important factors for lameness are the size of the fat pad in the heel (this dissipates force onto the hoof walls, and is linked to BCS) and the thickness of the sole.
What can you do? The importance of track condition, careful use of the backing gate, treating lame cows promptly are still critical. In addition, maintaining BCS will help cushion their feet with the fat pad in the heel. And a new concept to me – Conditioning heifers’ feet by gradually introducing them to walking on concrete before calving.

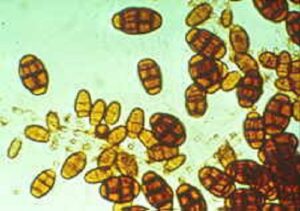
The pasture fungus Pithomyces charatarum multiplies and produces spores, which contain the toxin Sporidesmin. Sporidesmin causes injury to the liver. The bile ducts become thickened and may be completely blocked. The damaged liver cannot rid the body of wastes and a breakdownproduct of chlorophyll accumulates in the tissues and causes sensitivity to sunlight.
Sunlight causes immediate and severe skin inflammation to exposed parts of the body.The symptoms of FE therefore can vary from severe photo-sensitisation and in some cases death to sub-clinical effects on the production of meat, wool and milk. In any FE outbreak, many animals with liver damage show no clinical signs – but they suffer from subclinical FE.
Photosensitisation tends to occur about 2 weeks after exposure to spores and is characterised by irritation, reddening and oedema (puffiness) of exposed hairless or non-pigmented skin. This is followed by serum ooze and ultimately large sheets of skin may slough. Many animals affected by FE do not show outward signs; in fact only about 20% of animals with FE show skin signs. There will however, be some degree of liver damage and overall wellbeing will be compromised.
For rapid growth and spore formation the fungus needs warm, moist conditions common during the autumn. 4-5mm of rain or even heavy dews in conjunction with 2-4 nights when grass minimum temperatures remain above 12 degrees Celsius are sufficient to
initiate rapid increases in spore numbers. Spore counts rise even more rapidly when minimum temperature of the grass is high (15-16⁰C) and associated with high humidity and/or light rain. Generally it takes two or three such “danger” periods before spore numbers reach dangerous levels, each spore rise providing the base for the next increase in spore numbers. However prolonged periods of warm, humid weather early in the season can accelerate the onset of toxic pastures.
Predicting and identifying danger periods by monitoring spore countsThe control of FE includes:
- Spraying pastures with fungicide to prevent spore growth
- Administering zinc
- Cambridge Veterinary Services provides a daily spore count service through the eczema season. Grass samples are submitted to the clinic and results are reported to the owner the same day. The data is then collated as part of the ongoing monitoring service that we provide and is updated frequently on our website. Spore count information can be obtained by calling the clinic or from the website / Facebook page.
Prevention Options
Zinc can be administered in a number of ways:
Zinc sulphate through the water trough
- 60% effective
- Not very palatable – flavourants required
- Needs to be gradually introduced over time
- No access to alternative water sources
- Not suitable for providing protection in a “crisis” period
Zinc oxide oral drench
- 75-80% effective
- Zinc bullet
- 90% effective
- Great for young stock
- Slow release over a period of time
- Faceguard or Time Capsule
- Repeat administration required – usually 2-3 times in Waikato
Pasture Spraying
- Please contact us for details on this procedure eg how much zinc oxide to use for pasture spraying.
- Pasture spraying with fungicides including “Xspore” and new “Mycotak /Mycowet” system is also possible.
- This is the best option for owners of Alpacas.
- Please enquire about these Timecapsules
Faceguard Vs. Time Capsule
Both zinc bullets are inserted orally via a gun and sit within the rumen releasing a continuous, controlled amount of zinc over a period of time. It is highly effective and safe in most situations.
Time Capsules
Boluses contain compressed zinc oxide surrounded by a green shell of beeswax. The products come in a number of sizes according to the weight of the animal and requires repeat application every 4-5 weeks in cattle (4 weeks when counts are high) and will provide protection for six weeks in sheep and lambs.
The disadvantage with Time Capsules as you are probably aware, is the products fragility. If the green beeswax outing coating is damaged in any way the product cannot be used as there is a risk of zinc poisoning, which can be fatal.
Faceguard
Faceguard boluses contain compressed zinc metal.
In contrast to Time Capsules’, Faceguard bullets are extremely robust and can handle being dropped. They are less likely to cause toxicity issues compared to the Time Capsule (whose outer wax coating can be damaged by teeth at insertion which means it is digested faster and not provide protection for 4 weeks).
The faceguard bullet comes in only one size so if the animal is bigger then you adjust the number of bullets given. A special gun is used (different to the Time Capsule gun) and is loaded with more bullets for heavier calves rather than having to have several different sized heads with the Time Capsule. A maximum of 5 bullets can be inserted into the gun. A single treatment will last 6 weeks (as opposed to 4 weeks) and re-treatment can extend this out to either 10 or 12 weeks.
Cattle Zinc Drenching
Long Term Dosing Stabilised Drench eg Global Supa-Zinc
Mix 1 kg zinc oxide powder (Nu Zinc) with 1 litre of water (if not a stabilised
product add 200mls of stabiliser and 800 ml water).
• Mix water and stabiliser first if using.
• Sprinkle powder on the water and leave to settle and wet.
• Stir to a creamy paste.
• Daily dosing 3.5 mls per 100 kgs live weight
• 3-day dosing 13 mls per 100 kgs live weight.
• Weekly dosing 30 ml per 100 kgs live weight
Crisis dosing (only when spore counts are high), without previous long term dosing, gives less protection than long-term dosing and requires higher dose rates for protection over short periods. Stabilized drenches: 5ml/100kg live weight
Zinc Sulphate in drinking water
There are four main methods of adding zinc to the drinking water of cattle.
- Using an in-line dispenser to add a concentrated solution of zinc sulphate into the water reticulation system. Important points to remember:
• Set a level to which you will fill the reservoir containing concentrated zinc solution
• Adjust the dispenser or the reservoir volume to ensure that each day half to two thirds of its solution is injected into the water supply.
• Calculate the amount of zinc to be added each day (see table). Multiply the dose rate for each class of stock by the number then work out the daily requirement.
• At the same time each day add the total daily amount of Zinc Sulphate to the concentrate reservoir and then dilute with water to the FULL line. Stir to dissolve the zinc as you fill.
2. Adding Zinc Sulphate to a large tank (e.g. 22 000 litres, or 5 000 gals) which supplies the water reticulation system. The Zinc Sulphate is added to a large reservoir tank. The tank must contain at least 100 litres for every cow or cow equivalent. Remember the Zinc Sulphate should be added about the same time each day. Zinc Sulphate should be dissolved in water before adding to the tank.
3. Floating trough dispensers (Peta dispensers). Although not as reliable as the first two systems these still appear to give reasonable results and are ideal in situations with smaller numbers
4. Direct addition to the water trough – this will only cope with very small numbers of animals.
Note -1.The addition of Zinc Sulphate to the water supply is only suitable to long-term routine dosing – it is not suited to crisis dosing during danger periods. Make sure zinc is only distributed to stock. Household and shed water needs to be kept separate. Make sure that livestock do not have access to alternative fresh water during the period that zinc is being added.
Addition to the water may be unreliable for treating animals not milking.
2. Mixing of other products in water (eg nutrimol) can reduce effectiveness by settling out the zinc in water lines. This may eventually block the lines and severe FE may result.
How to start:
Cows should be introduced to increasing zinc concentrations in water over a period of about 3-5 days.
There are two forms of zinc sulphate available; heptahydrate is commonly available, monohydrate is more concentrated and is used at 2/3 the dose of heptahydrate.
Troughs on the reticulated system in paddocks that have not been grazed should be primed with zinc sulphate at the rate of 1g/L (0.7g monohydrate per litre).
Once calibrated a volumetric measure is sufficiently accurate for regular use. Weigh out the required zinc sulphate into a plastic bucket. Level the surface and mark the height, fill the bucket to this level each day.
Concentrated zinc sulphate solutions are caustic. Avoid direct contact and wear protective goggles.
Be sure to follow the mixing instructions with all zinc products, in particular adding mono-zinc to water not the water to the powder.
Take home message
FE is a debilitating disease of livestock that can be largely prevented through knowledge of the disease and prophylactic administration of zinc at strategic times of the year. Start monitoring spore counts in December and institute preventative measures when conditions favour the proliferation of spores. If in doubt, be sure to contact your veterinarian to discuss the right approach for your animals.
DEER
Red deer are more susceptible to FE than cattle. Fallow deer are more susceptible than sheep so they need more protection than Reds.
Prevention options include:
Spraying pastures with fungicide – Regular spraying with fungicides provides the most appropriate control method for preventing FE in deer. Start the spraying programme early while spore counts are low.
Zinc – the effectiveness and safety of zinc as a prevention has not been researched. If used, dose rates as for sheep (Fallow deer) and cattle (Red deer) should be followed. Because of low water intake, zinc in drinking water is not highly effective but will help in some situations.
Provide supplementary feed – such as hay, silage, meal or crop
SHEEP
Grazing Management
Planned grazing can substantially reduce the risk of FE in hill country. Good planning is essential and it must start months in advance.
Identify the safe areas on your farm and aim to have a feed bank on these areas for the FE season. The best way to identify the safer areas on your farm is by regular spore counting over several years – but in the meantime the shady south facing faces are generally safest.
The spores are concentrated in the litter at the base of the pasture so the harder the sheep
graze the greater the risk of FE.
Try to minimise the number of young stock retained to late summer and autumn.
Breeding for Resistance in Rams
Tolerance to FE is strongly inherited so sourcing rams tolerant to FE will reduce the susceptibility of their offspring to FE
Sheep can be dosed at twice weekly, weekly or fortnightly intervals with Zinc Oxide. However the longer the interval, the lower the level of protection. Salmonellosis has been
associated with fortnightly dosing so if this is a potential problem shorter intervals are recommended. Watch for diseases like pink eye and pneumonia, which may also develop due to frequent yarding.
RECOMMENDED DOSE RATES:
Stabilised drench – 0.5ml/1 0kg LW x interval (days) (recipes for mixing these drenches are in the cattle section).
GOATS
Goats are generally more resistant than sheep and their browsing habits make them less prone to ingesting spores. Milking goats are probably at greatest risk. Prevention is best achieved by never making stock graze into the base level of pastures. The fungus grows on the litter at the base of the pasture and the spores are concentrated there. Other options include:
Spray pasture with fungicide
Provide supplementary feed (crops, fodder, hay, silage)
Zinc prevention – in highly toxic conditions use zinc oxide as for sheep
Mycoplasma update (May 2018)
We now have a positive farm confirmed in the Cambridge area, and several Waikato farms are under Movement Restriction and testing after NAIT movement tracing. The government will be announcing the national policy on Monday 28/5/18.
Commercial tests are now available; PCR tests for bull sheath scrapes, and for milk. These tests can yield both false positive or false negative results (it is a very frustrating disease!). Please contact the clinic if you would like to discuss these options.
Mycoplasma is spread primarily via direct contact from cow to cow (even over the fence) as the bacteria are found on the nose, respiratory tract, mammary gland, vagina and prepuce and transmitted in secretions such as milk, tears and semen.
Biosecurity is nonetheless vitally important to prevent transmission between farms on boots, equipment etc.
Remember disinfection is a 2 step process – first scrub to remove all the organic material, then disinfect!
Both testing and culling are now ongoing as well as continued surveillance. It is important that we maintain vigilance.
Keep an eye out for the signs:
- Swollen joints and lameness in cows
Cows still quite bright
Mastitis that does not respond to antibiotics
Abortion and birth of weak calves
Arthritis in calves
Pneumonia in calves
Middle ear infection in calves leading to a head tilt, and conjunctivitis
Mycoplasma are bacteria that do not have cell walls, so many antibiotics do not work, and they are difficult to culture in samples. The disease is common worldwide, but no evidence of its presence was found in NZ in 2007 when 244 bulk milk vats were tested. There is no human health risk or threat to trade.
Mastitis
Put simply, mastitis refers to inflammation of the mammary gland (udder). Mastitis is generally considered the most costly production disease of dairy cows. It affects the farmer financially in several ways;
- Discarded milk
- Veterinary and drug costs
- Increased culling
- Reduced production for the remainder of the season due to permanent damage to the secretory tissue
- Penalties in milk price due to changes in milk quality and elevations in somatic cell count
- Most inhibitory substance grades are caused by intramammary antibiotics.
Classification of Mastitis
For purposes of defining the source of infection, mastitis is classified as contagious mastitis or environmental mastitis. Contagious mastitis results from bacteria that are transmitted from cow to cow i.e. the bacteria are present on the udder of cows. Environmental mastitis originates from bacteria in the cow’s environment, i.e. a contaminated paddock.
Mastitis is also classified as clinical mastitis (disease with visible changes in the milk) and subclinical mastitis (disease that is not visibly apparent). The great majority of cases are subclinical. Because it is not obvious, dairy producers may not be aware of subclinical mastitis and the extent of lost milk production that results. Undetected subclinical mastitis can also be a source of infection to other cows, will elevate Somatic Cell Count (SCC) and decrease production.
Clinical mastitis is characterised by the following;
- Rapid onset, heat, swelling, reddening, or hardening of infected quarters. This is painful.
- Visible abnormalities in milk, including clots, flakes, or discolouration.
- In acute cases systemic signs, including fever, anorexia and reduced rumination, dehydration, weakness, depression, and noticeable decline in milk production.
- The cow may be lame due to swelling of the udder
Subclinical mastitis is characterised by the following;
- No visible change in the udder or in appearance of the cow
- No visible abnormalities in milk
- Reduced milk yield in the affected quarter(s)
- In some cases, periodic episodes of clinical mastitis in affected cows
- Elevated Somatic Cell Count (SCC) and Bulk Tank Somatic Cell Count (BTSCC)
Acute mastitis: refers to sudden onset with severe clinical signs
Chronic mastitis: persistent or recurrent with mild or no clinical signs
Gangrenous (black) mastitis – This is caused by certain bacteria that produce nasty toxins restricting blood flow to the affected quarter. This results in a blue/ black quarter that is cold to the touch. The toxins from the bacteria and the dying udder tissue are absorbed into the body and consequently these cows become severely ill and often go down. Antibiotics are usually unsuccessful as they have no effect on toxins. The majority of animals with black mastitis are euthanized or die.
Structure of the Udder and Milk Synthesis
The udder is derived from a highly modified sweat gland. Milk is produced by small, sac-like structures deep within the tissue called alveoli. Each milk producing cell is surround by muscle, which when stimulated by oxytocin, contracts and squeezes milk into the gland. The milk then flows into the cistern and down the teat.
Milk synthesis is a complex process that involves the rumen, liver and udder. The liver produces glucose from products of remen fermentation. The glucose is transported to the udder where it is converted into lactose. The amount of lactose in the milke controls milks volume.
Milk protein & casein is also made in the udder from components of rumen fermentation. Milk protein concentration is determined by the amount of energy rather than the protein in the diet. Milk fat is synthesized in the udder as well. The components are derived from the fermentation of fibre in the diet, bypass fat and the mobilisation of body fat (during early lactation). Adequate fiber is therefore essential for milk fat production.
How does mastitis affect milk synthesis and quality?
When the udder becomes infected and inflamed there is significant injury and damage to the milk producing cells of the udder. The cow’s immune system responds to the infection by sending billions of white blood cells (pus) into the udder. It is the white blood cells that make up 98% of the somatic cell count. Infection = increase in SCC. In addition to this influx of cells, there are significant changes in milk composition such as decreased lactose, protein and fat and increased salt. Several enzymes leak into the milk from the damaged cells. This leads to rapid breakdown and rancidity of milk.
The influx of cells that occurs with infection provides a measure of milk quality and can be assessed by either counting them in 1000’s per milk or using the Rapid Mastitis test (RMT – see notes). Similarly the increased salt concentration improves the conductivity of milk and is the principle for electronic mastitis testers.
As a result of all these changes, milk from cows with mastitis is not suitable for the production of certain products and for this reason the dairy companies have payment incentives and penalties in place.
Major Mastitis Players in New Zealand
The majority of mastitis is caused by 2 different species of bacteria; Streptococcus uberis & Staphylococcus aureus.
Coliforms (E. coli), Strep agalactiae & Strep dysgalactiae occasionally cause mastitis.
Streptococcus uberis
- This is the most important mastitis pathogen in the pastoral dairying systems of NZ
- Environmental mastitis
- Most infections occur during the early dry period and in the first 6 weeks after calving
- Very sensitive to penicillin being 95% effective and therefore good cure rates
- Subclinical infections are uncommon
- SCC are not as high as with staphylococcus infections
- Main cause of heifer mastitis
Detection of Mastitis
The early detection and treatment of all quarters with clinical mastitis reduces the risk of severe mastitis developing, reduces the likelihood of infection being spread from cow-cow and reduces the risk of an increase in BMSCC.
Methods of Detection:
- Visual
- Changes in the behaviour of the animal; slow to walk in, lame, kicking cups off
- Changes in the milk; watery, blood, clots or flecks
- Changes in the udder; hot, swollen, asymmetrical, tender
- Clots on the filter sock
- SCC
- Individual SCC (herd test results) are very useful for detecting subclinical mastitis and chronically infected cows
Rapid Mastitis Test (RMT)
- Used to identify which quarter/s is involved, screening for milk quality, SCC after calving before putting cow’s milk into the vat
- Electronic Mastitis Test (Conductivity Meters)
- Works on the salt levels within the milk. Many are available. Care is required with interpretation.
When to Use each Test
After Calving – After the compulsory withholding period of 8 milkings, test cows with RMT or mastitis meter before adding their milk to the vat. Heifers may take up to 10 days before SCC is down and RMT is negative. Introducing heifers into the too early after calving is often the reason for getting high SCC grades early in the season when milk volume is low
High Bulk Somatic Cell Count – strip all cows before cupping to find infected quarter/s. If nothing detected, use RMT or conductivity meter on whole herd
Herd Test Results – used to identify high SCC cows. Use RMT or conductivity meter to then identify affected quarter/s
Control and Prevention of Mastitis
Pre-Calving Management
Cows are very susceptible to infection around calving because their natural defense mechanisms are low. New infections occur, and subclinical infections which have persisted through the dry period may flare up into clinical cases. Induced cows are even more vulnerable to mastitis infections because their immune systems have reduced efficiency at that time.
Around calving, the udder is often filled with milk for relatively long periods without the flushing effect of being milked. Bacteria may enter the end of the teat, particularly if high udder pressure opens the teat canals. They can then multiply and establish infections. High numbers of environmental mastitis bacteria may contaminate teats, especially if udders are wet and exposed to mud and manure. This can happen easily when cows and heifers are on the ground during calving.
Because of the high incidence of mastitis in the first month after calving, special care in this period will pay off.
Draft springing cows (transition cows) into a separate mob
Give a bigger break to avoid pugging and contaminating the environment
Need to feed well above maintenance to allow for the rapidly growing foetus. Introduce some of the feed that will be given after calving, to give the rumen flora time to adjust to the new diet
Any cow or heifer really tight and dripping milk can be milked just enough to take the pressure off. Teat spray thoroughly afterwards
Once calved, separate immediately from calf and milk out properly
Oxytocin can be used if animals are reluctant to let their milk go after a few milkings, or in case of mastitis. It will aid in milk let-down and emptying of the glands.
Lactation Management
Avoid pre-washing teats unless very badly soiled
Keep hands clean. Wear gloves! Bacteria live within the cracks of milkers hands and are transferred from cow-to-cow. Bacteria are far less likely to survive on latex
Teat Spray
Apply at every milking for the entire season. It is one of the most effective cell count and mastitis control measures available, if applied correctly
To be effective the spray needs to be applied as soon after cup removal as possible
Failure to cover the whole teat of every cow at every milking is the most common error in teat disinfection
Use a high concentration (30%) of emollient during the first few months to prevent cracking which can harbour bacteria
Treating Cows
Mastitis cows should always be kept separate from the herd, and milked and treated last. A cluster that has been on a mastitis cow can potentially infect the next 8 cows being milked on that cluster!
Disinfect cluster and hands before moving to next cow
Milking Machines
Get machines checked at least once a year. Teat end damage, black pock, sore and teat end eversion are signs there may be issues with the milking machine or milking management.
Dry Cow Therapy
The most effective way to treat contagious Staph mastitis
Reduces dry cow mastitis to virtually zero
It is now compulsory for farmers to have an annual Dry Cow Consultation with their veterinarian who will help you decide which product to use and which cows to treat
Culling
Strategic culling of repeat offenders
R.M.T. Guide and Instructions
Most intramammary infections are subclinical therefore clinical examination of quarters cannot be used to differentiate between infected and non-infected quarters. The Rapid Mastitis Test (RMT) is a quick, cheap & simple test that can be conducted cow-side to help detect subclinical mastitis.
Test Procedure
- Direct 2-2 squirts of millk from each qaurter into the appropriate section on the paddle
- Add equal parts of RMT reagent and gently mix by swirling for about 10 seconds
Reading the Test
- A positive reaction from a subclinical quarter/s will form a slime/gel. The greater the inflammation the thicker the slime
- Milk containing a cell count of 1 million/ml or more will turn the test sample to a thick jelly
- RMT tests conducted on treated quarters may show positive results for a week after a successful treatment
- NB: The RMT test is a subjective measure of subclinical mastitis. What I may call a 3 a second observer may call a 2. The accuracy of the result will improve if the same person is performing the test regularly.
- Recording the Test (see over)
- Quarters with scores of 2-3 require treatment
- Reading Score Meaning
No slime 0 Normal and healthy
Slime 1 Slight thickening which disappears with paddle movement
Thick Slime 2 Infected quarter
Heavy Slime/Clot 3 Heavily infected
An outbreak of nitrate poisoning is a terrible scene to behold – a group of cows lying dead on the ground, with several more staggering around, and abortions anticipated from a number of the survivors. This is a genuine emergency where immediate veterinary treatment is needed. So what, specifically, should you look out for?
- Laboured breathing with gasping
- Chocolate coloured blood and mucous membranes
- Pale, brown, grey or blue mucous membranes (e.g. the eye)
- Muscle tremors, weakness and stumbling gait
- Collapse, depression, convulsions
- Death can occur within 30 minutes
Normally, nitrate is converted to nitrite and then to ammonia by the bacteria in the rumen. But if there is excess nitrate, nitrite is absorbed into the bloodstream, where it converts the haemoglobin in red blood cells to methaemoglobin. This form cannot carry oxygen, so the poor ruminant (and the foetus if she is pregnant) is starved of oxygen, resulting in the above signs around 4-5 hours after eating the problem feed.
Soil nitrate is taken up by plants, and then used for the production of protein. However, problems can arise if the plant accumulates too much nitrate because the plant does not have enough energy. Low light is a critical factor, especially dull, overcast weather. Plant nitrate peaks early in the day and decreases towards afternoon.
Over application of nitrogen fertilisers, sewage sludge and farmyard manure may also lead to excess nitrate accumulation. It seems to take 10-14 days for nitrate levels to peak after the application of fertilizer, and if the growth conditions are optimal, levels should be safe to graze after 16-21 days.
The prime risk situation is rapid plant growth in highly nitrogenous soils.
High risk stages are young plants (e.g. new seeding), and in re-growth, especially in the roots, stems and stalks.
There is an intravenous treatment available. This is a veterinary product, and must be given at the correct dose, or it may cause more problems!
Preventative measures include:
- Submit pasture samples to assess nitrate levels and risk.
- Knowing which plants / paddocks are most often culprits.
- Restrict grazing on suspect crops.
- Delay grazing animals after fertiliser application.
- Feed cows hay, silage or mature grass first to avoid gorging on suspect paddocks.
- Carbohydrate helps animals convert nitrates (e.g. maize silage).
- Put stock on feed in late morning / early afternoon at least 4 hours before dark.
- Remove stock from feed and call us immediately should you see any signs.
The common and highly contagious disease infectious keratoconjunctivitis (pinkeye) can affect cattle at any age causing considerable pain and distress with significant economic losses due to reduced weight gain or weight loss.
How do cattle get infected?
- A major predisposing factor in the development of pinkeye is damage to the cornea. This typically arises due to dust, long grass or plant pollens. The resulting damage then allows the bacteria, Moraxella Bovis to colonise the irritated area and start to multiply producing the characteristic signs of pink eye. Flies then feed on the secretions and spread disease from one animal to another.
What do we see?
- Typically, affected animals develop a photophobia so they are squinting their eyes, the eyelids are often in spasm and there is a discharge staining the face. As the disease progresses, an ulcer starts to develop on the centre of the cornea surrounded by a ring of inflammation. The cornea develops oedema which gives it a blue appearance interfering with vision. In severe cases the cornea can perforate.
Treatment
- The cornerstone of treatment involves the administration of antibiotics either directly to the eye or locally. Antibiotic powders have been used widely in the past but have now fallen into disfavour due to the irritation caused by placing powders in the eye. Antibiotic eye ointment is a simple and effective means of treating mild to moderate cases. Early treatment will minimise the risk of permanent scarring to the cornea and reduced weight loss associated with pain. In more severe cases, the vet may opt for an ‘eye flap’ – temporary surgical closure of the eyelids in addition to medical treatment.
Prevention and Control
- Control flies by using products that are licensed for fly control in cattle
- Avoid grazing calves on long pasture
- Avoid overcrowding
- Remove affected animals from the main mob
- Treat early
- Consider vaccination of healthy animals in known hot spots
Pinkeye in Sheep
- Pinkeye is also a very common ailment afflicting sheep and goats however, unlike cattle, the pathogen implicated in disease is a Chlamydia species as opposed to Moraxella. Outbreaks in NZ are generally mild and occur annually in adult sheep during summer and autumn. As with the disease in cattle, infection is spread indirectly by dust, pollen in grass and flies which have been contaminated by the secretions of infected sheep. Handling of the face and head of sheep when drenching may be an important means of spread. Treatment, if required, generally involves the use of oxytetracycline sprays or ointments.
Drench
There are several ways to accidentally poison stock with drench that you need to be aware of.
Pour-on is deadly if given by mouth. Overdosing by more than 50% is dangerous, especially with Levamisole or Selenium. There are no Abamectin (Ivomec-type) products licensed for oral use in cattle because of potential for overdosing. Never add drench to bulk tanks such as calf milk feeders as you will have no control over how much each animal drinks.
Always read directions and dose rates carefully, and if you have delegated drenching to other staff, make sure they fully understand your instructions, route of administration, and the dose rates.
Bloat Drench is extremely toxic to calves in it’s concentrate form. Never use old bloat drench drums as calf feeders.
Plants / Trees
- Oleander is extremely toxic, to stock and to people. In one case, 5 leaves killed 5 calves. Remove it with extreme care as scratches can also cause problems.
- Yew leaves, bark and seeds are all poisonous, and just as bad fresh or wilted. Do not throw trimmings into stock paddocks.
- Acorns are particularly poisonous when they are green (fallen during high winds). Calves suckling cows that have eaten acorns are most susceptible, followed by calves eating them, then adult animals.
- Rhododendron has been responsible for the death of several pet lambs, leading to great distress. Keep lambs out of the garden, and trimmings out of the paddock.
- Lily of the Valley contains digitalis glycosides, the same toxin found in foxglove. Once again, keep it away from stock.
Other plants
There are plenty of other plants that can cause poisonings in stock, including Poa Aquatica (which has locally been known as Oreipunga disease due to its occurrence in this area), rhubarb, arum lily, macrocarpa (particularly after trimming or high winds), ragwort, tutu, hemlock, bracken fern, marijuana, and many others. Most will only be poisonous if eaten in large quantities but are better not to be eaten at all.
Rubbish / Dump Sites
Old car batteries and sheep dip have caused problems due to the lead and arsenic content. Beware the rubbish pile and inquisitive stock.
If you are concerned that your stock has eaten or been overdosed with any of the above, or you are unsure of how safe a product or plant matter is, please ring the clinic immediately on 0800 226 838 or (07) 827 7099 and ask to speak to a vet.
Cambridge Veterinary Services offers both manual and ultrasound pregnancy testing services for cattle, and ultrasound pregnancy testing for alpacas. We have trained operators with proven experience and equipment. We can combine testing with reproductive analysis to ensure you know how your herd is performing.
Why Pregnancy Test?
Pregnancy testing of cattle is a very useful management tool. Different approaches will be required depending on the management situation and what you wish to know. It allows you to achieve many goals if done at the right time.
Which method?
In situations of small numbers of cows, we will almost always use manual pregnancy testing, because it is faster, and because the ultrasound equipment is expensive and requires adequate restraint of the cow. Manual pregnancy testing also requires good facilities for the safety of people and cattle. A strong cow race is a minimum requirement, a headbale is better.
There is much debate on which method you should use. As far as accuracy is concerned they are both fairly even as long as the tester is experienced. They both have limitations in that they will only accurately date pregnancies between 6 and 16 weeks. After this time they both fail to see enough of the uterus to be very accurate for dating.
There is a very small risk of rectal rupture with scanning that does not exist with manual testing. Both can be done at the same speed if you are well organised. Cows will tend to strain more following manual testing. All cows scanned empty should be checked manually before being culled. We will do this as we scan the cows. Accurate recording of results is vital and empty cows should be permanently marked. Good tag numbers are essential.
Timing – The Best option
- Alpacas can be ultrasound pregnancy tested from 4 weeks up to four months. Adequate facilities are required, talk to your vet.
- Scanning can be done 6 weeks after mating in cattle. For manual and ultrasound testing we prefer to wait 8 weeks before confirming cows are empty.
One off whole herd testing
If whole herd testing is done eight weeks after the end of mating it is possible to remove all empty cows. This prevents the costly burden of carrying empty animals through the winter. This is especially so if you are looking for culls in a dry summer. It can be difficult to give accurate calving dates at this stage if mating started several months before as most of the pregnancies will be too advanced. This goes for scanning as well as manual palpation. We simply cannot size the pregnancy accurately after 16 weeks.
Heifers too?
It is also a valuable exercise to pregnancy test heifers. This allows earlier heifers or those in calf to AB to be sorted from later or bull mated heifers. Late heifers may be culled early or selected for sale. Again timing is important to ensure you get the most out of it.
Purchased stock
Finally any stock you buy should either be tested before purchase and certified in calf or tested once you get them home with right of return if empty. An empty cow isn’t worth much on the hooks compared with an incalf one in your herd! Make sure you check these cows.
Please note that research has shown a consistent occurrence of 2-5% foetal resorption before 12 weeks of pregnancy in cattle which is not related to pregnancy testing. After 12 weeks this drops to 0.5%
1-2% loss of pregnancy (slips) is accepted as normal in dairy herds.
Salmonella is a significant disease of cattle and sheep and it is increasing in prevalence. Usually striking without warning and spreading rapidly, the effects of Salmonella are devastating. Moreover, it can make you, your family and your staff very sick too. Since 2014 there has been a marked increase in S. bovismorbificans in cows and calves, from a handful of cases to 281 in 2019. Illness and death rates have been seen of up to 46% & 8% in dairy herds and 75% & 50% in calves. There has also been a rise in human cases, and some in sheep. Several sheep farms sharing a river saw salmonella enteritis and deaths after shearing in 2019, possibly due to contaminated water and stress.
S. bovismorbificans outbreaks in people have been associated with sprouted seeds and salads, so they are potentially adapted to soil and watery habitats. Some isolates in Australian sheep have also displayed hypervirulence, where the bacteria become more infectious and lethal after passage through an animal.
Salmonella is spread by healthy carrier animals which don’t show signs of disease, but shed bacteria (usually intermittently or at low levels). These bacteria go on to infect other animals. Carrier animals can shed Salmonella for months or even years. It is spread by infected materials (e.g. faeces, aborted materials) which can be further spread by
scavenging animals such as seagulls or hawks. Salmonella can survive in the environment for a long period of time (e.g. months to years in ideal conditions like wet paddocks, or dry, shaded areas such as cattle or sheep yards). Conversely, it can be killed in days with freezing or heating.
Strains of Salmonella
Cattle
- Brandenburg (primarily causes abortions)
- Typhimurium (primarily affects the gut)
- Bovismorbificans(primarily affects the gut)
Sheep
- Hindmarsh (primarily affects the gut)
- Brandenburg (primarily causes abortions)
Irrespective of the strain, all types of Salmonella
can cause outbreaks and deaths (5% in cattle and sheep).
Outbreaks happen when ingestion of an infective dose of Salmonella occurs at the same time as stress and a change in feed type or quality. Stress can be caused by stock movement or handling, bad weather, or calving/lambing. Usually, Salmonella would already be circulating or being shed at low levels in the flock/herd, but the diet change causes a change in the animals’ gut
environment (for example, an increase in pH or reduced production of volatile fatty acids). This reduces the number of bacteria that need to be ingested to cause illness and/or increases the number of Salmonella shed by carrier animals.
At the same time, stress, late pregnancy or immune suppression make the animals less able to fight off infection. It is at this time that animals become sick or abort; sick animals shed more Salmonella into the environment,
which can infect other naïve flock/herd mates, perpetuating the outbreak.
Environmental conditions (such as wet weather) may also contribute, as it will favour Salmonella survival in the
environment and/or help spread Salmonella around. Removal of aborted material is essential as this a good source of bacteria
The most common way Salmonella is introduced to a farm is through healthy looking carrier animals (cattle, sheep etc.).
Higher risk practices include:
- Off-farm grazing
- Intensive feeding
- Purchasing/leasing stock
- Shared boundaries/stock yards
So, reduce risk by:
- Minimise time off feed when yarding/transporting
- Clean and disinfect yards between groups of animals
- Separate stress events
- Control pests and scavengers
- Vaccinate at-risk animals prior to stress events or diet changes
- Double check Magnesium supplementation forms/ rates (cattle)
The recent NZ Vet Journal had a whole issue on the TABA epidemic. Here are a few highlights gleaned from the MPI and Massey authors:
Theileria orientalis was first reported in NZ in 1984, but the anaemia epidemic spanned from August 2012 to March 2014. In the first 18 months there were 496 case herds (reported to MPI); 79% were dairy and 21% beef.
Of 882 individual cases (submitted) 93% were positive for Theileria orientalis Ikeda. This is a protozoan parasite. There are 10 other types of T. orientalis, 3 of which have been found in NZ (chitose , buffeli and type 5). Chitose occasionally causes anaemia. Australia and Japan have also been significantly affected by Theileria orientalis, although it is found worldwide.
Theileria is carried and transmitted by the cattle tick Haemaphysalis longicornis. The larvae, nymphs and adults all feed on ruminants, but different individuals. The infection is not passed onto the tick eggs. A tick can pick up the parasite from the blood of an infected cow, and then pass it on to the next cow it feeds from. The tick-borne parasite is a protozoan, and the piroplasm form causes destruction of red blood cells, leading to anaemia. Animals can recover from infection, but the parasites may persist possibly for life; periods of stress such as calving can lead to a relapse. Disease is more frequently seen when naïve animals are introduced into an endemic area, or when infected animals are introduced to properties with ticks. The ticks are found throughout the North Island, plus Nelson and Golden Bay, and TABA has only occurred in tick areas.
Some interesting figures: Incidence risk 1%, cumulative mortality 0.23%, case fatality rate 17%.
It is believed the epidemic’s origin was the importation of infected cattle. There appear to be two scenarios of Theileria spreading. Firstly via cattle movements: farms that had Theileria were more likely to have brought cattle onto the farm, and from a greater distance. Trucking in infected cattle to a naive area would probably initiate each of these local outbreaks. Obviously the peak movement of 500,000 cattle happens on June 1st, leading to the mixing of infected and naïve cattle and ticks, and spread of the disease. Then a second localized spread via tick vectors: cases were seen in clusters within 20-30 days and up to 15-20km from a case farm. Infected tick nymphs can be carried to neighbouring properties by wildlife such as hares, horses, deer, dogs, goats and sheep. 100 ticks have been noted on the ears of a hare!
The time period from infection by tick bite to the parasite being found in the bloodstream is 10 days, and the number of bugs increase to 30-40 days, which is when the animal has the most severe anaemia and clinical signs. The peak of TABA in October 2013 therefore probably arose from infection soon after calving via the re-emergence of over-wintered nymphs. By the time you see a cow sick from it, she has been infectious to ticks for over a month already!
Beef calves were at greater risk of TABA than dairy calves, and calves were the most affected age group in Northland. This is probably because beef calves are born later (coinciding with the peak questing period of overwintered nymphs), dairy calves are housed for the first few weeks, and tick density is higher in Northland with earlier resumption of tick activity. Data from Africa suggests that as an area becomes endemically stable, the incidence of obvious disease falls and is often restricted to young animals; this may explain why there was lower risk of disease in Northland. In contrast, the Waikato bore the brunt of TABA with adult dairy cattle.
The prediction is that some areas will reach endemic stability (with clinical disease not being seen much as ticks and theileria are a constant factor), but that epidemics (outbreaks of disease) may continue in areas of marginal tick habitat. Practical treatments still focus around pasture management, tick control, animal husbandry (minimizing stress), supportive therapy and, if needed, blood transfusion. Buparvaquone is effective but the with-holding is too long to be practical. Some research work for a potential vaccine was being done in Japan.
Cattle and sheep cannot be transported:
- With an injured udder or mastitis,
- in late pregnancy (and give birth within 24 hrs),
- with eye cancer that is >2cm or bleeding, or if they are lame
- With ingrown horns or horns that may cause injury
SHEEP AND BEEF
- Mulesing sheep is prohibited
- Local anaesthetic must be used if castrating with a high tension band (not a rubber ring) or at over 6 months of age
- Do not allow horns to become ingrown
DAIRY CATTLE
- Do not allow horns to become ingrown
- Inserting objects into cows for milk let-down is prohibited
- Removing any part of a cow’s tail is now prohibited
- Do not use a goad to strike or prod livestock in sensitive areas
- Local anaesthetic must be used for disbudding or dehorning
LIFESTYLE BLOCKS
- Shelter – make sure your animals have appropriate shelter (dry, shaded, ventilated, clean, big enough, food and water nearby)
- Dogs on the backs of utes must be secured so they cannot fall off
- It is best not to tether your goat for long periods, but collars and tethers must fit so the animal can eat, drink, breathe and pant and does not cause injury.
- Castration
- Equipment must fit, be clean, and not cause injury
- Transporting calves – if the ute / deck is higher than 90cm, loading facilities are required.
Welfare 2016
- Bobby calves must be fed, kept in suitable shelter, and handled with due care. As of next year, a ramp must be available for them to walk up to the truck.
- Euthanasia by blunt force trauma is not allowed. Personnel must be trained and competent to use a firearm or captive bolt.
- Hip lifters are to be removed if the cow cannot promptly support her own weight.
- Cows must not be transported where her weight is taken entirely by the hip clamps/vehicle.
- Cows supported in a sling must be able to breathe freely, not suffer unnecessary discomfort, and be lowered if they are not supporting their own weight within one hour.
- If they are still recumbent after 48 hours, a vet examination is recommended – we can check for dislocated hips or other diagnosis, give a prognosis, or feedback on welfare.
- Animals must be fit for Transport. Calves must be at least 4 days old, healthy, able to stand with a dry navel and fed within 2 hours. Adult cattle must be bearing weight evenly on all 4 legs; if they are lame or have any health issue, a vet may issue a certificate only if they meet certain criteria.
- Milk letdown must not be stimulated by insertion of water or air into the vagina.
- It is best practice to have an Animal Health Plan written in consultation with your vet. This provides an opportunity to go over husbandry skills, to plan ahead, and formalize decision trees for mastitis, lameness, calvings and recumbent cows for example.
Leptospirosis
Leptospirosis is the disease every farm should vaccinate for. It is caused by bacteria (leptospires) which can be carried by cattle and sheep even if they look healthy. The bacteria colonize the kidneys, which means it is spread via urine. Even tiny droplets can gain access to the human body via mucous membranes (mouth, eyes, nose) and cuts to the skin. If you can smell urine you can catch it! It can also be caught from contaminated effluent, stagnant water etc. so be aware of water-borne transmission via ponds etc.
Symptoms
- Cattle – redwater, abortion, generally unwell
- People – flu like symptoms, aches, pains, fever/chills, Nausea/vomiting/diarrhoea. Some people will be more seriously affected, and may need to be hospitalised due to Liver damage, Kidney failure, Brain swelling, Heart failure
- Treatment – hospitalization, antibiotics
Prevention
- Hygiene – it is really important that you do not smoke, eat or drink during milkingas this is a great way to introduce the infection. Gloves should be worn and other PPE as appropriate. Hands should be washed regularly. These precautions should also be applied when hosing effluent in shed and yard, and calving cows / handling membranes. Cuts and scratches should be covered with waterproof plasters.
Ponds and waterways should be fenced off from stock. Effluent should not be spread in wet conditions, leptospires can last for 6 months, and pasture should not be grazed until effluent has dried. Prevent effluent and water settling especially near the shed by clearing drains, culverts etc. - Pest control – rats can also carry lepto, ensure there is a policy
- Pigs – don’t have them, or vaccinate them and keep effluent contained
- Dogs should be vaccinated
- Vaccination – the national vaccination strategy has reduced the incidence of leptospirosis in dairy cows and farmers (although beef and abattoir workers are still at risk). Calves need 2 injections for the primary course, thereafter most animals get a booster in the winter. There are many strains or types of lepto, but the vaccine covers the most common ones.
Salmonella
Salmonella is another well known disease which can be caught from animals and can be vaccinated for.
Again it is a bacterial infection which can be carried by apparently healthy animals, but this one is spread in the faeces not the urine. It Lives in the guts of many species, and can cause bloody diarrhoea, milk drop and death.
It can affect both calves and adult cattle.
Prevention is by vaccination of the herd, and personal hygiene. Wearing gloves and washing hands are not just useful for covid! Again there are multiple strains, and birds can carry it too, but cow effluent / calf scours are the biggest risks. Contaminated and improperly cooked poultry is also a risk.
Treatment is generally antibiotic injections.
Ringworm
Ringworm is actually a fungal infection like athletes foot! In cattle it is highly contagious and can spread rapidly within a mob, particularly youngstock. Generally, the cow’s immune system gets rid of it after a few months, but it looks unsightly. Kittens are also a common source of ringworm spreading to children as they cuddle them. Cattle show multiple grey, flat, hairless circles on the head and neck. Direct transfer from a cow can leave a person with the classic scaly round lesions on your arms with a red edge. If you suspect it, tell your doctor you work with animals.
Treatment for people is an anti-fungal cream or tablets, but we do not treat cattle.
Prevention is…awareness and hygiene!
Bill Hancock
Peter Briston

Cecilia van Velsen

Julie Hetherington

Patrick Taylor

Kelvin Scown
Product Manager